Hospitals and clinics are expected to be sterile environments, but they face a constant battle with medical facility contamination. This persistent, global challenge can turn these places of healing into potential sources of infection.
The Hidden Sources of Contamination
Contamination in a medical setting is rarely the result of a single failure. Instead, it usually stems from a complex interplay of environmental factors, human behaviour, and the resilience of microscopic pathogens. To effectively fight contamination, administrators and infection control specialists must identify exactly where the threats are hiding.
The Persistence of Pathogens
The primary culprits are the microorganisms themselves. Bacteria, viruses, fungi, and spores can survive on surfaces for surprisingly long periods. “Superbugs” like MRSA (Methicillin-resistant Staphylococcus aureus) and C. diff (Clostridioides difficile) are particularly notorious because they have developed resistance to standard antibiotics and many cleaning agents. These pathogens can linger on bed rails, privacy curtains, and waiting room chairs, waiting to be transferred to a susceptible host.
High-Touch Surfaces and Equipment
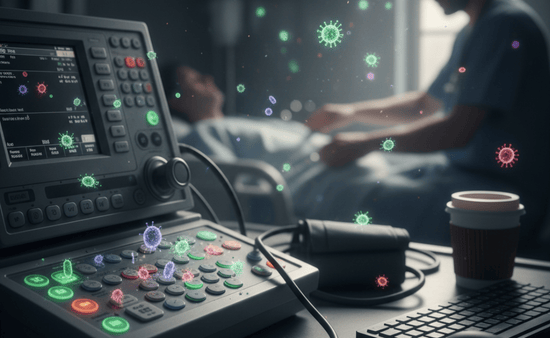
It is easy to assume that contamination is mostly found in operating rooms or waste disposal areas, but the most common vectors are often the most mundane objects. High-touch surfaces—doorknobs, light switches, elevator buttons, and keyboards—are frequent reservoirs for germs.
Furthermore, medical equipment itself can become a vector if not properly sterilized between uses. Items like stethoscopes, blood pressure cuffs, and IV poles move from room to room, potentially carrying bacteria with them. More complex devices, such as endoscopes or ventilators, require intricate cleaning processes; if any step is missed, the risk of cross-contamination skyrockets.
The Human Element
Despite the best protocols, human error remains a significant source of contamination. This does not necessarily mean negligence; often, it is a result of high-pressure environments where staff are rushed. Missed hand hygiene opportunities, improper donning and doffing of Personal Protective Equipment (PPE), or a simple failure to follow a specific cleaning sequence can inadvertently spread pathogens. Visitors, too, play a role, as they may bring in outside germs without realizing the strict hygiene standards required in a clinical setting.
The Impact on Patient Health and Recovery
The consequences of contamination extend far beyond a dirty room. When a patient contracts an infection while receiving medical treatment, the trajectory of their recovery changes drastically.
The physical toll is the most immediate concern. Patients with compromised immune systems—such as those undergoing chemotherapy, the elderly, or premature infants—are particularly vulnerable. An infection that might be a minor nuisance to a healthy person can become life-threatening for these individuals. Sepsis, pneumonia, and surgical site infections are common complications arising from contaminated environments.
Beyond the physical impact, there is a psychological toll. Patients trust healthcare facilities to be safe havens. When that trust is broken through an acquired infection, it can lead to anxiety and a loss of confidence in the healthcare system.
From an administrative perspective, the impact is also economic. HAIs lead to readmissions and extended hospital stays, costing the healthcare industry billions of dollars annually. Resources that should be focused on new treatments are instead diverted to managing preventable infections.
Strategies for Prevention and Control

Combatting medical facility contamination requires a multi-layered approach. There is no “silver bullet,” so facilities must rely on a combination of strict protocols, specialized services, and education.
Rigorous Cleaning Protocols
Standard janitorial cleaning is insufficient for medical environments. Facilities must adhere to protocols that distinguish between cleaning (removing visible dirt), disinfecting (killing most germs), and sterilizing (eliminating all microbial life).
Environmental services staff must follow strict schedules, using hospital-grade disinfectants approved by regulatory bodies like the EPA. Every surface must be treated with the appropriate chemical for the correct “contact time” to ensure pathogens are destroyed.
In situations involving hazardous biological materials or significant infectious outbreaks, standard staff may not have the resources to handle the cleanup safely. In these instances, facilities may contract specialized biohazard cleanup services like those available in Salt Lake City to ensure that the area is remediated according to the highest safety standards. These specialized teams are trained to handle dangerous pathogens and ensure that the environment is returned to a safe state without putting hospital staff at risk.
Sterilization of Medical Instruments
For invasive procedures, sterilization is non-negotiable. Autoclaves, which use high-pressure steam, are the industry standard for surgical tools. Chemical sterilization is used for heat-sensitive equipment. Beyond the machinery, the tracking of these tools is vital. Modern facilities use barcode systems to track every instrument from the sterilization room to the patient, ensuring that no step in the safety chain is skipped.
Staff Training and Hygiene Culture
Technology and chemicals are useless without a culture of safety. Hand hygiene remains the single most effective way to prevent the spread of infection. Hospitals employ “secret shoppers” to monitor hand-washing compliance and use visual reminders at every bedside.
Training also extends to the proper use of PPE. Staff must be drilled on how to remove gloves and gowns without contaminating themselves, a process that requires focus and practice.
The Role of Technology in Hygiene
As the threat of contamination evolves, so does the technology designed to fight it. Healthcare facilities are increasingly turning to automated solutions to supplement human cleaning efforts.
UV-C Light Disinfection
One of the most prominent advancements is the use of Ultraviolet-C (UV-C) light. Mobile robots can be wheeled into patient rooms after manual cleaning is complete. These robots emit high-intensity UV-C light that destroys the DNA of bacteria and viruses, reaching nooks and crannies that a human cleaner might miss. It provides a final, powerful layer of defense before a new patient is admitted.
Antimicrobial Surfaces
Materials science is also playing a role. We are seeing a rise in the use of antimicrobial surfaces—materials infused with copper or silver ions that naturally kill bacteria upon contact. Integrating these materials into bed rails, countertops, and door handles provides a passive, continuous form of disinfection that works 24/7.
Air Filtration Systems
Airborne contamination is a major concern, particularly for respiratory viruses. Modern hospitals are retrofitting HVAC systems with HEPA (High-Efficiency Particulate Air) filters that trap microscopic particles. Negative pressure rooms are used to isolate patients with contagious airborne diseases, ensuring that contaminated air does not escape into the corridors.
Conclusion
The battle against medical facility contamination is never truly “won”; it is managed. As pathogens evolve and adapt, so too must our strategies for containment and cleanliness. It requires a commitment from every level of the healthcare hierarchy, from the hospital CEO investing in new sterilization technology to the visitor remembering to sanitize their hands at the door.

